The way we work
We aim to provide a smooth intake, diagnostics and treatment process. We use MAAS Medical Interview (Crijnen & Kraan, 1985), an evidence based format for medical interviewing, and (child)psychiatric assessment according to the standards (Hengeveld & Schudel, 2003; Lindauer & Staal, 2022). We use the concept of a honeycomb inside a beehive, the Inner Development Goals and Theory U as inspiration for continuous integration of our internal processing and interaction with those asking for advice or help. We are part of a learning network to ensure continued education and learning as professionals and as a team (see under Quality). Treatments that we apply are based on evidence-based concepts and have been scientifically proven to be valid and reliable.
Initial assessment is done by the (child and adolescent)psychiatrist and a psychologist or psychotherapist, and an intern (master student psychology) is sitting in taking notes. After a multidisciplinary meeting we offer a first advice meeting. Further diagnostics may be done by a psychologist, psychotherapist or orthopedagoge together with the intern apart from the (child)psychiatrist. After further diagnostics a second advice meeting takes place in which the treatment plan is discussed. Treatment can be provided by a parental management guide, a psychologist, family therapist, art therapist, psychomotor (child)therapist, sensorimotor integration/physiotherapist, child and adolescent dietician, paediatrician, (child and adolescent) psychiatrist and/or trauma-sensitive yogatherapist. We also collaborate with the local sportschool and the local stable with riding school if indicated. We aim to have regular evaluation meetings (once every 3-6 months for children, once every 6-12 months for adults).
We may work individually with the child, parent or adult patient, but mostly collaborate within the multidisciplinary team to create optimal results for patient and family.
We focus on wellbeing, empowerment, improvement of self-esteem, attachment as well as reduction of ACEs, psychopathology and physical complaints in a systematic way.
Infographic ACEs 3 fysieke gezondheid
We try to enhance the efficacy and resilience of the patient and expect that patient, whether child or parent or adult, commits to his or her therapy to get the most out of it. This includes e.g. filling out questionnaires, homework exercises, dairy writing, e-health modules, sticking to diet lists, sports/activities, music or art work, coming in for therapy sessions, collaborating in diagnostics or family sessions, etc.
Parents should be prepared that we expect them to reflect upon their own upbringing and way to raise their children as well as their own functioning and interaction, as children are always influenced by their parents. It is not just the child that needs to change or whose problems are focus of attention. Often family dynamics or the relationship between parents, or parents’ management style has to change as well. When adolescents are 16 years of age they have an independent treatment agreement with us, but we value involvement of parents and other family members in all cases to overcome dysfunctional family dynamics and to increase empowerment and social support.
We collaborate closely and have regular multidisciplinary meetings and evaluations.
We expect patients, their family, relatives, friends and other visitors to adhere to our house rules. Please click on the picture or link to read them in English or Dutch.2022 Huisregels_iMindU BV2022 Houserules_iMindU BV
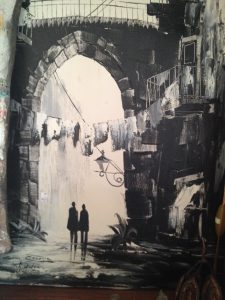
We have transformed from a solutions-oriented mindset to a “soulutions”-oriented mindset. This implies alignment of the head, heart and hands. We strive to induce such a mindset in the people we work with in accordance with the Inner Development Goals to collectively reach the Sustainable Development Goals.